1. What is the problem?
"Medicine is a science of uncertainty and an art of probability." —William Osler
Uncertainty is inherent in medicine. No matter how far we pursue medical knowledge—whether due to deficiency, controversy, conflict, or confusion—uncertainty will always remain a part of every medical decision (Figure). Reduction of uncertainty is a quintessential aspect of medicine, but complete elimination of uncertainty is impossible[1]. As physicians it is essential to accept the limits of our knowledge and the uncertainty associated with those limits. However, there is little science or teaching on how to respond when faced with the all too common question, "But, Doctor, how can you be sure?" Chalking this up to the "art of medicine," every physician must independently develop his or her own approach for how to respond to such a question. We assert that systematically refining our approach to managing uncertainty has the potential to improve the patient experience while simultaneously helping to repair some of the greatest problems with our current healthcare delivery model.
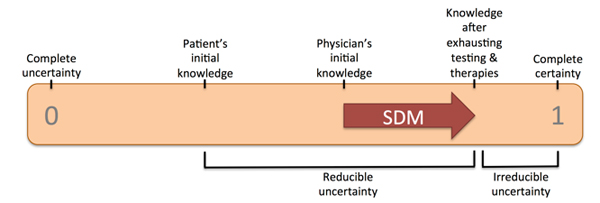
Much of the overuse in our healthcare system can be attributed to our inability as physicians to effectively manage uncertainty, i.e., a futile attempt to mitigate uncertainty [2]. Effective communication of uncertainty will be required for maximally efficient stewardship of resources in a post-fee-for-service era, where physicians in the United States will no longer be compensated simply for doing more. Shared decision-making (SDM) has been offered as a means to engage patients and improve transparency thereby addressing these concerns [3,4]. If SDM is going to deliver on its promise to improve care and reduce overuse, it will be essential to develop a systematic approach to effectively managing uncertainty. In order to accomplish this, physicians must be able to understand and communicate uncertainty to their patients. Presently, however, physicians are poorly equipped for the task. Although uncertainty surrounding medical decisions is based on a probabilistic framework, medical education has traditionally focused on categorical thinking characterized by flow diagrams, binary decisions, and absolutes. In fact, it is physicians with graduate degrees in other fields—perhaps due to the additional statistical training—who appear more willing to disclose and discuss uncertainty with their patients [5].
Deficiencies in knowledge regarding the interplay of diagnostic testing and uncertainty appear to contribute significantly to overuse. In a zealous attempt at placing the signs, symptoms, and diagnostic test results of patients into discrete disease categories of certainty, physicians frequently fail to recognize they have crossed a line where further testing has more risk than benefit. This testing threshold varies depending on the risks and benefits associated with the test, the understanding of which requires a good grasp of probability theory and decision analysis. Similarly, when making treatment decisions, an appreciation for the implications of the therapeutic threshold are necessary. Without training in these areas, physicians will not be able to effectively convey these considerations to patients and involve them in an informed, SDM process.
 © 2015 Works & Days Quarterly and Ted Melnick
© 2015 Works & Days Quarterly and Ted Melnick